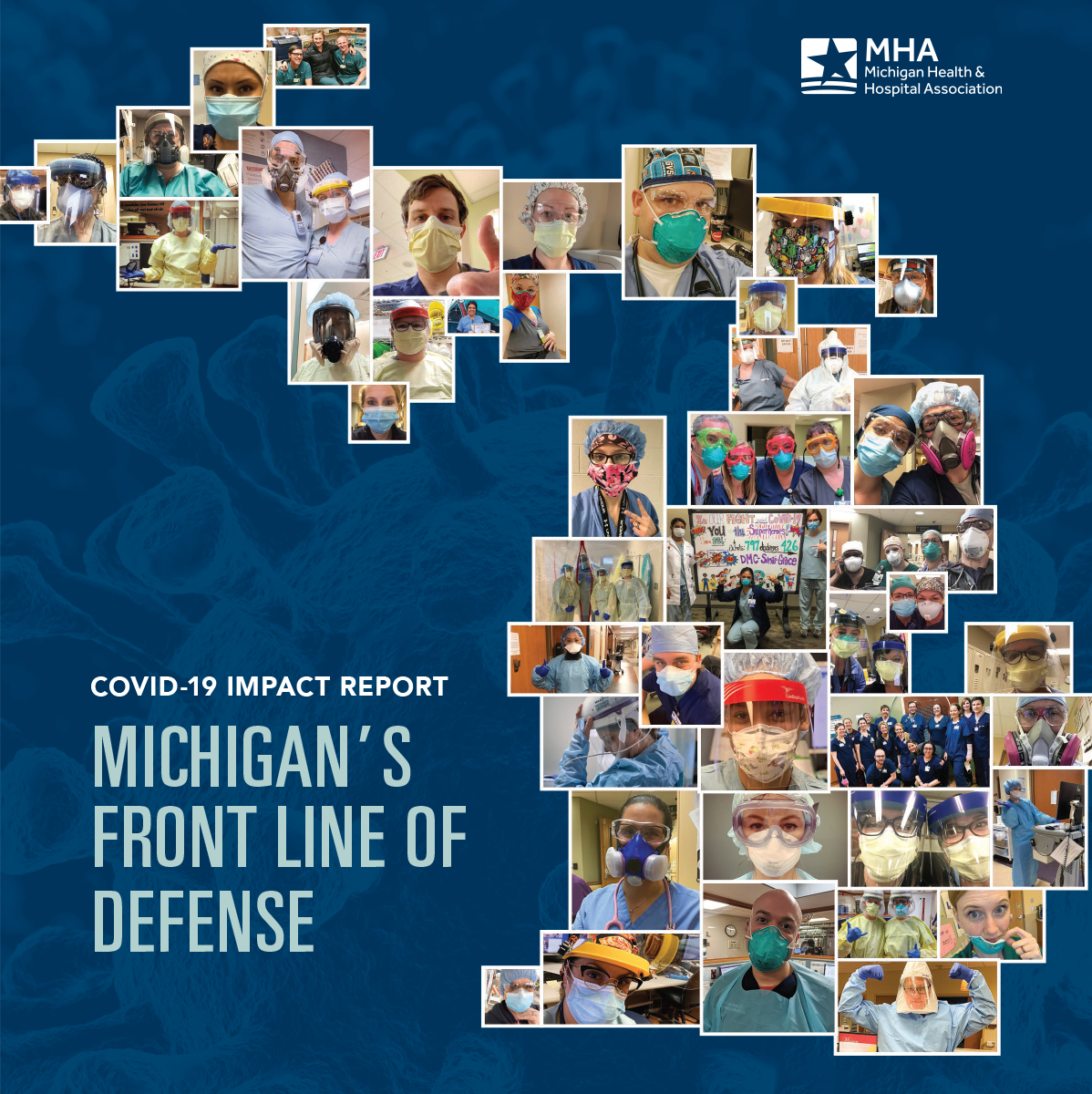
Michigan’s Front Line of Defense
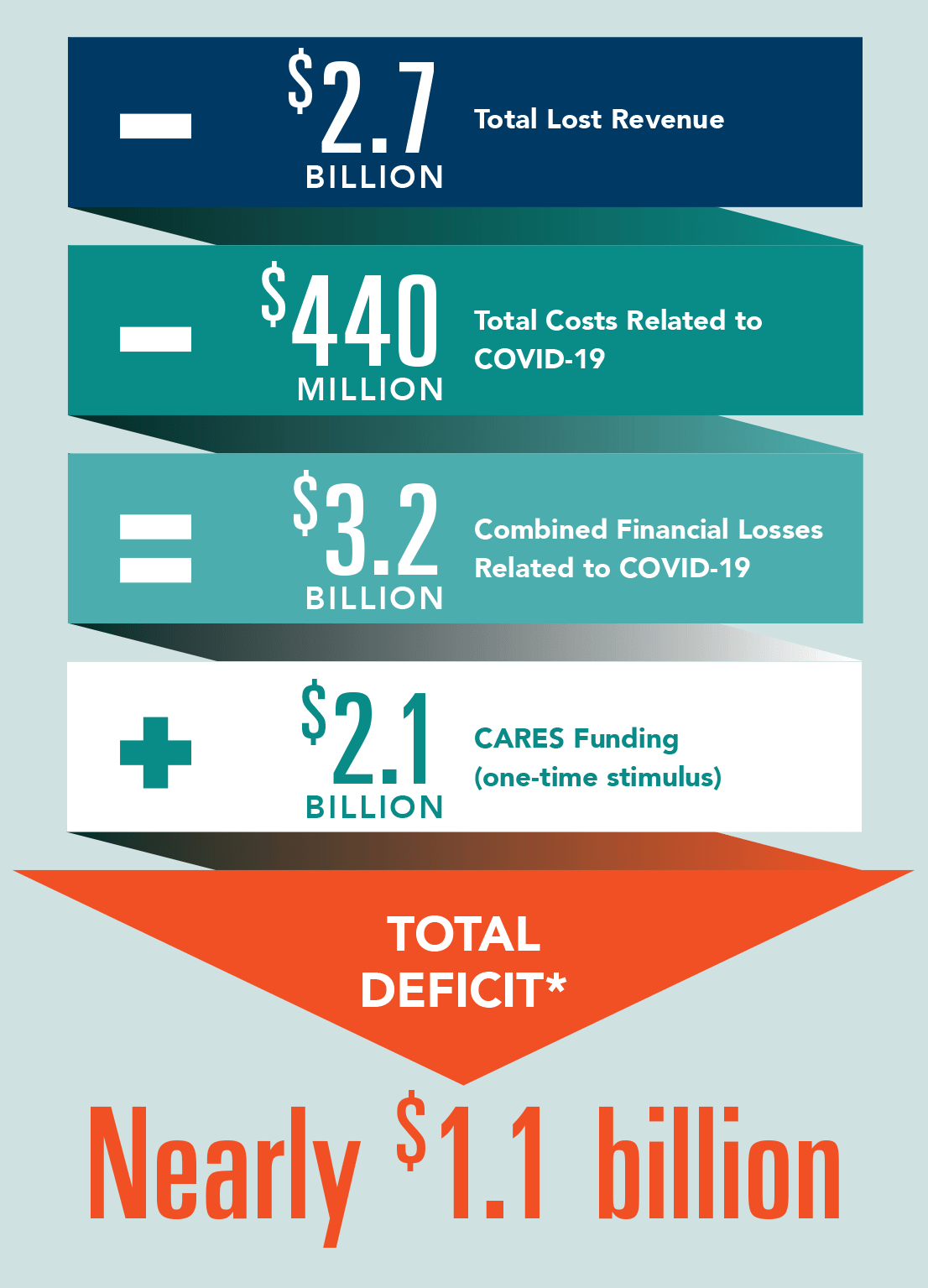
The COVID-19 Impact Report, Michigan’s Front Line of Defense, highlights how hospitals have responded to the pandemic and the severe COVID-19-related financial losses they’ve suffered. In total, Michigan hospitals have suffered COVID-19 related financial losses that are nearing $3.2 billion and a financial deficit of nearly $1.1 billion, which continues to grow as hospitals respond to the COVID-19 pandemic.
Despite the challenges our hospitals faced such as procuring enough personal protective equipment (PPE), increasing testing capacity and changing care delivery models, hospitals and their staff persevered to flatten the curve in Michigan.
The reports also highlights testimonials of patients around the state from healthcare heroes who continue to work around the clock to save lives as COVID-19 impacts our communities.
Data for this report was voluntarily submitted by participating hospitals and health systems to the Michigan Health & Hospital Association from March through mid-June 2020.
COVID-19 in Michigan
Beginning in March 2020, hospitals across Michigan implemented emergency preparedness plans in preparation to treat COVID-19 patients. Thousands of patients required hospitalization and many more needed testing, with Michigan’s healthcare workforce serving as the front line of defense against the COVID-19 pandemic. While caseloads have varied across the state, the impact has been felt by every hospital and health system.
Testing
Widespread testing is vital in identifying, treating and containing COVID-19 outbreaks. As of July 12, hospital labs have conducted over 400,000 COVID-19 polymerase chain reaction (PCR) tests and average 7,000 tests per day.
PPE
COVID-19 created global demand for PPE that has never been seen before. To protect patients and staff, hospitals purchased PPE at exponentially higher rates at a total cost exceeding $93 million and counting. According to MHA estimations, at the height of the pandemic in April, Michigan hospitals every day were using:


36,000 N95 Masks

1.53 Million Gloves

330,000 Surgical Masks

46,000 Surgical Gowns

20,000 Face Shields
Treatment
Hospitals increased general and intensive care unit (ICU) bed capacity, developed COVID-19-only units and refurbished existing facilities to improve infection prevention and treatment. Together, these efforts helped hospitals save lives and prevent infection spread.

During the peak surge, Michigan hospitals cared for 4,700 COVID-19 patients April 10, including 1,700 COVID-19 patients in ICU.
Since the end of the data collection, more than 16,000 patients have been discharged from Michigan hospitals.
The Financial Cost of COVID-19
COVID-19 has had a significant financial impact on hospitals, including in exponential costs associated with preparing for a surge of patients, delaying nonemergency care for months and treating an increasing population of unemployed patients who have lost private insurance coverage. Hospitals already operated on thin operating margins, and they provide $188 million in financial assistance to vulnerable populations. In total, hospitals have experienced losses nearing $3.2 billion.
*Costs are based on data voluntarily submitted by participating hospitals and health systems to the MHA during March, April, May and most of June 2020. Published figures are likely on the low-end of financial loss estimates for Michigan.
Impacting Communities Across Michigan
The pandemic has physically and mentally impacted the entire healthcare workforce. Exposure to and contraction of COVID-19 led to hundreds of personnel being placed on leave. As staff physically recover, many more struggle with feelings of stress, grief and loss. Hospitals are working to address these challenges. In the meantime, healthcare heroes across the state continue to report to work every day to care for their patients and their community.
“The loss in revenue we experienced has been great and we, like so many hospital systems, need and depend on the support from the state. While we are not necessarily considered a “hot spot” where we are located, it is state support that will help hospitals and health systems get back on their feet. Our communities depend on us, and, now more than ever, hospitals need to recalibrate and be prepared to survive whatever the next chapter may bring.”
-Diane Postler-Slattery, PhD, FACHE, President and CEO, MidMichigan Health

“The nurses and staff at the hospital kept a close watch on me and went above and beyond to ensure I was comfortable. To see everyone lined up and down the hallway while I was being released was an amazing feeling.”
-Alex Ewing, a 32-year-old Mackinac Island resident who spent three weeks on a ventilator and nearly a month at McLaren Northern Michigan before being discharged.

“I wouldn’t even have known if the hospital was busy or anything else because they got me upstairs so quickly. Everyone was just really on top of things and I could tell they were taking precautions.”
-Frank Bono, bone marrow transplant recipient, who received specialized care while hospitalized for five days with COVID-19-related symptoms before being discharged by the Karmanos Cancer Institute in Detroit.